After age 40, many people begin to lose bone density more quickly. Bones that once were robust now require extra attention to maintain strength, prevent fractures and slow down deterioration. Whether you’re a man or a woman, this decade is a key window for preserving skeletal health. We’ll explore what happens to bone health after 40, why it matters, and walk you step by step through diet, exercise, lifestyle, screening and medical considerations to keep your bones strong.





What Happens to Bone Health After 40
Bone Remodeling & Age
Bones are living tissues constantly undergoing remodeling — old bone is broken down and replaced by new bone. But after about age 40, this balance tilts: less new bone is laid down to replace what’s removed. (OrthoInfo)
Accelerated Loss in Midlife
For women especially, the perimenopausal and early menopausal years (mid-40s to 50s) can bring an acceleration of bone loss due to declining estrogen levels. One source noted women can lose up to 20% of bone mass in the first five years after menopause. (El Camino Health)
Peak Bone Mass & Why 40 Matters
The stronger the bones you built earlier in life, the better “reserve” you’ll have. After 40, you may not build much new bone, so preserving what you have becomes crucial. (Holland Hospital)
The Risk of Osteopenia and Osteoporosis
“Low bone mass” (osteopenia) can progress to osteoporosis if unchecked — resulting in fragile bones and higher fracture risk. (PMC)
Why Improving Bone Health After 40 Is Important
- Fracture risk: Weak bones lead to increased risk of fractures of hip, spine, wrist, etc. (Endocrine)
- Quality of life: Fractures may limit mobility, independence and overall wellbeing. (PMC)
- Healthcare costs & burden: Preventing bone loss helps reduce future medical issues. (PMC)
- Longevity of musculoskeletal strength: Maintaining bones supports muscles, joints and general functional capacity.
- It’s never too late: Even if you didn’t focus on bone health earlier, midlife is still a pivotal time to act. (Holland Hospital)
Key Areas to Focus On
Here are the major domains you’ll work on: exercise, nutrition, lifestyle (including habits), screening/medical, home & fall-prevention. Let’s dive into each.
1. Exercise: The Foundation of Bone Strength
Physical activity is one of the strongest influences on bone health.
Weight-bearing & impact exercise
Activities where your feet/legs bear your weight — walking briskly, jogging, dancing, stair climbing — stimulate bone remodeling. (OrthoInfo)
Aim for at least 30 minutes a day, 4 or more days per week. (OrthoInfo)
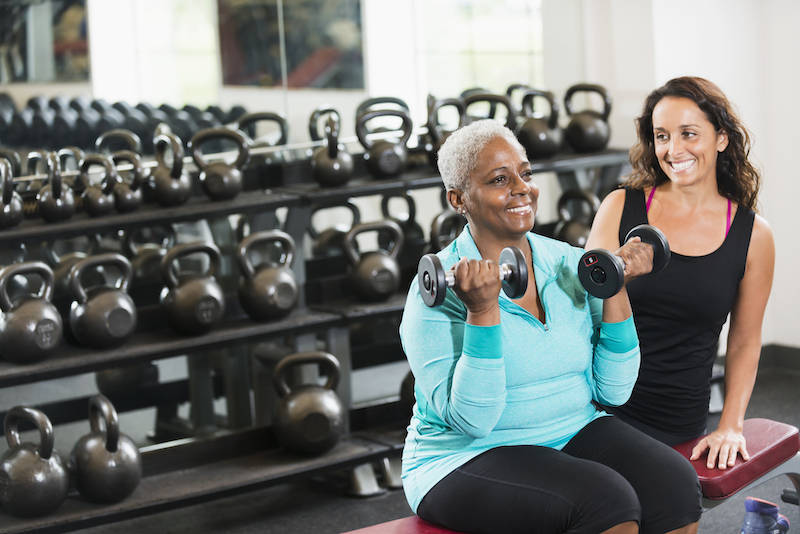
Resistance / strength training
Using free weights, machines, resistance bands or bodyweight moves (squats, lunges, push-ups) helps your muscles pull on bones, promoting bone formation and strength. (nhs.uk)
Include at least 2 days per week focusing on major muscle groups.
Balance and mobility training
Improving balance reduces fall risk — a major component of fracture prevention. Tai chi, single-leg stands, heel-to-toe walking, yoga all help. (Holland Hospital)
How to integrate in your day
- Choose a mix of walking, stair climbing, and weight training
- Start gradually if you’re new: e.g., 10 min walking, plus 15 min strength, then build
- Make it a habit: schedule sessions like appointments
- Adapt exercises if you have joint issues — consult a physiotherapist or certified trainer if needed








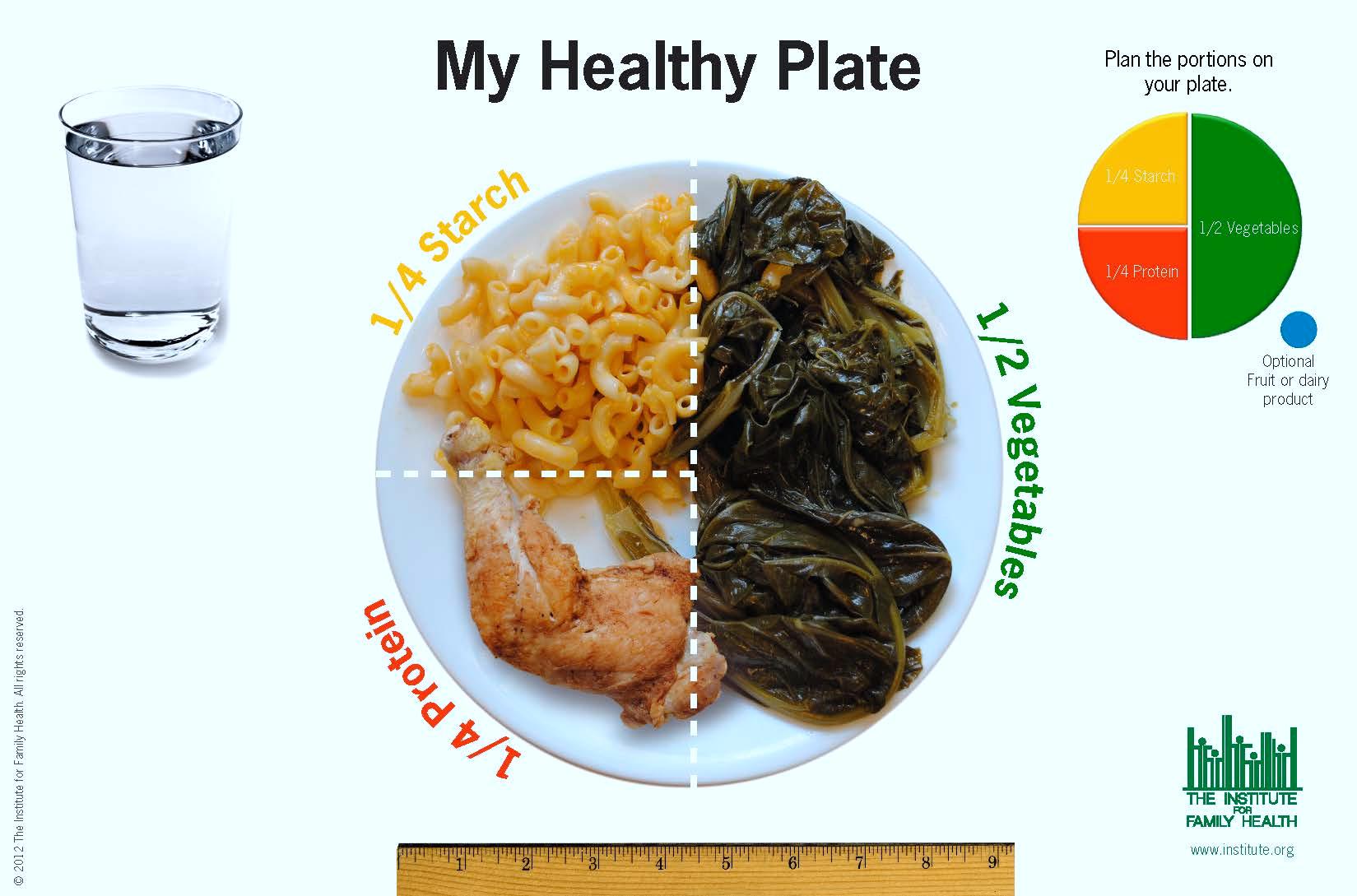
2. Nutrition: What to Eat for Bone Health
Diet plays a foundational role. Here are key nutrients and tips.
Calcium
Your bones need calcium to remain strong. After 40, adults generally need about 1,000 mg per day; for many women at or past menopause, 1,200 mg is recommended. (El Camino Health)
Good sources: low-fat dairy (milk, yogurt, cheese), fortified plant milks/cereals, leafy greens (kale, broccoli), sardines, tofu with calcium. (Holland Hospital)
Vitamin D
Vitamin D helps your body absorb calcium. Without enough vitamin D, dietary calcium may not be effectively used. (Endocrine)
Sources: sunshine (skin production), fatty fish (salmon, mackerel), egg yolks, fortified foods, supplements if needed.
Protein
Adequate protein supports bone and muscle health. As you age, you may need slightly more than the standard minimum to preserve muscle mass, which in turn supports bones. (Verywell Health)
Other minerals & nutrients
Magnesium, potassium, vitamin K, and trace minerals (zinc, copper) all play roles in bone metabolism. Include nuts, seeds, whole grains, legumes, vegetables. (Verywell Health)
Lifestyle diet factors to watch
- Limit excess salt, caffeine and soft drinks — these can interfere with calcium balance. (Holland Hospital)
- Moderate alcohol consumption — heavy drinking is linked to bone loss.
- Avoid very low-calorie diets or rapid weight loss without professional supervision, as they may harm bone mass.








3. Lifestyle Habits That Support Bone Health
Avoid smoking
Smoking is a risk factor for bone loss and fractures.
Limit alcohol
Excess alcohol intake weakens bone and increases fall risk.
Maintain healthy body weight
Being underweight is a risk for bone loss; obesity has its own risks (joint wear, fall risk). Aim for a healthy BMI and body composition.
Ensure adequate sleep & manage stress
Poor sleep and chronic stress may interfere with bone metabolism indirectly (via hormones, physical activity reduction, poor diet).
Sun exposure and safe vitamin D synthesis
Get moderate sun exposure (while protecting skin) to help vitamin D synthesis.
4. Screening, Medical & Professional Considerations
Bone density testing
If you’re 40 or older and have risk factors (family history of osteoporosis, prior fracture, long-term steroid use, early menopause, low body weight), discuss bone mineral density testing (e.g., DXA scan) with your doctor. (Penn State Health News)
Risk stratification and medical therapies
Especially for women entering menopause or men with low testosterone, hormone changes can impact bone. Hormone therapy, bisphosphonates and other medications may be options in consultation with your physician. (Endocrine)
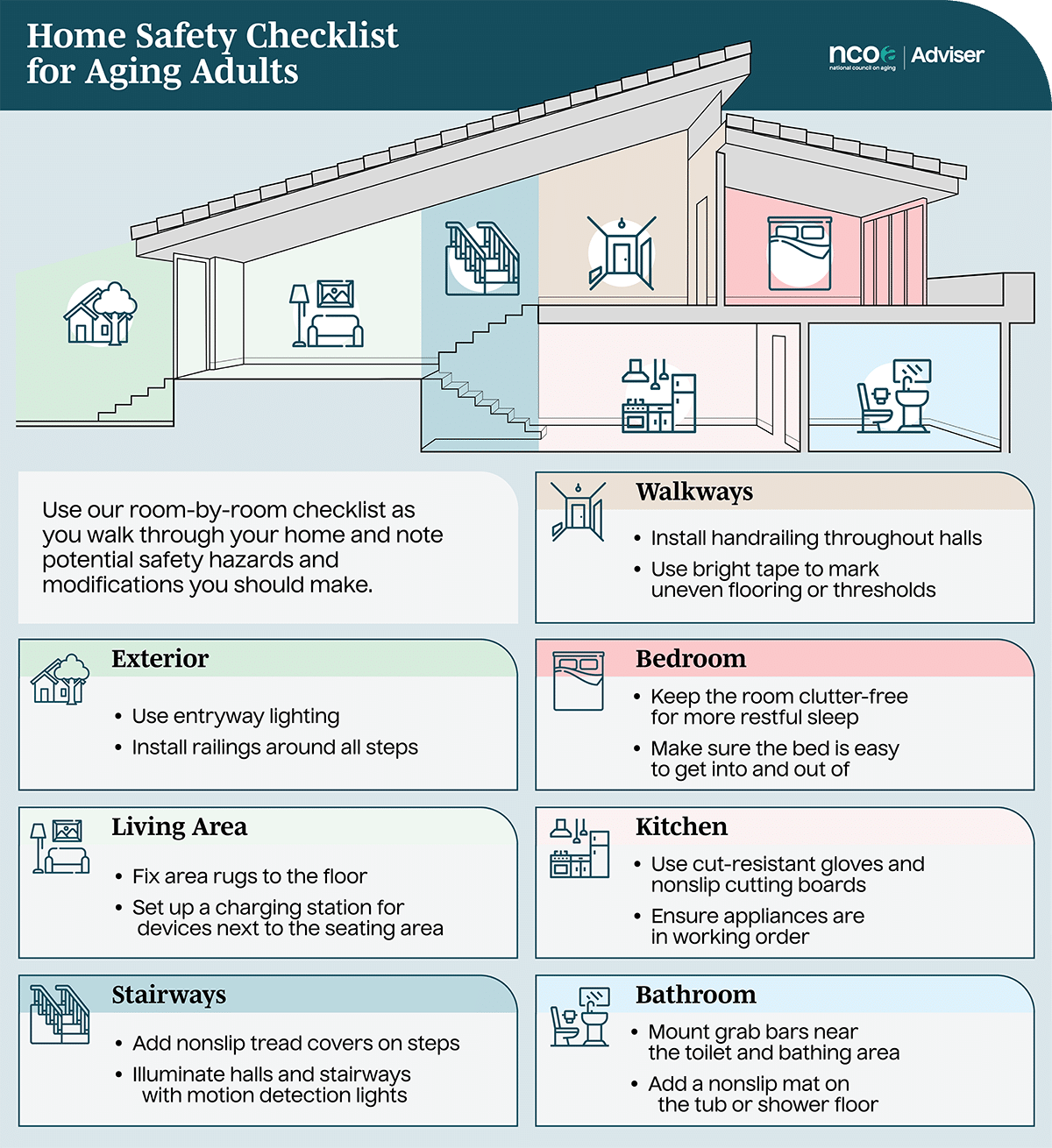
Fall-risk assessment
At age 40+ it’s helpful to evaluate fall risk (balance issues, medications, environment) and mitigate it proactively.
Review medications & health conditions
Some medications (e.g., glucocorticoids, anticonvulsants) and conditions (hyperthyroidism, celiac disease) increase bone loss risk. Make sure your provider is aware.
5. Home Environment & Fall Prevention
Given that weaker bones + falls = fractures, optimizing your home and habits matters.
- Remove tripping hazards (loose rugs, clutter, cords)
- Ensure good lighting, especially at night
- Use handrails on stairs or slippery areas
- Incorporate strength and balance training into your daily routine
- Choose supportive footwear
- If vision or hearing are impaired, address these as they contribute to fall risk









Special Considerations for Men and Women
Women
- Perimenopausal decline in estrogen accelerates bone loss. (El Camino Health)
- After menopause, bone loss can be rapid; hence proactive habits in the 40s are especially beneficial.
- Hormone replacement therapy (HRT) may be discussed with your doctor for bone protection, depending on individual risk/benefit. (Endocrine)
Men
- Men lose bone mass more slowly, but after 40 bone-loss still matters especially if they have risk factors (low testosterone, steroid use, family history).
- Do not assume bone health is less important — muscle strength and bone strength go hand-in-hand for fall and fracture prevention.
Putting It All Together: A Practical Action Plan
Here’s a sample plan you can adapt, with timelines and milestones:
Week 1–4: Baseline & Habit Setup
- Get baseline measurements: weight, body composition (optional), bone health discussion with doctor.
- Start a walking program: 20–30 minutes brisk walking, 4 times per week.
- Add one resistance training session/week (light weights or bodyweight).
- Review diet: ensure at least 1,000 mg calcium/day, get plenty of leafy greens, fatty fish.
- Review home environment for safety.
Month 2–3: Build & Expand
- Increase resistance training to 2 days/week; each session 30 minutes focusing on legs, back, hips, arms.
- Add balance training once per week (e.g., tai chi class or simple balance drills).
- Monitor diet; ensure vitamin D intake (sun exposure plus food/supplements as needed).
- Quit or reduce smoking/alcohol if applicable.
Month 4–6: Optimize & Review
- Continue walking, resistance and balance training. Try adding impact weight-bearing (e.g., dancing, stair climbing, light jogging if comfortable).
- Meet with your doctor to discuss whether bone density testing is appropriate or whether any supplement/medication is needed.
- Re-assess diet and lifestyle: Are you getting enough protein? Are you controlling salt/caffeine/alcohol?
- Check home/fall safety again.
Ongoing: Maintenance and Monitoring
- Maintain exercise routine for life; bone health is lifelong.
- Re-visit screening every 2–3 years or sooner if risk changes.
- If fractures or falls occur, talk to your provider about bone specialist referral.
- Adjust diet and activity as you age (60s, 70s) since bone loss risk increases.
Common Myths & Misconceptions
- Myth: “My bones are fine because I have no pain.” — Truth: Bone loss is often silent until a fracture occurs. (PMC)
- Myth: “Only women after 50 should worry about bones.” — Truth: Bone health after 40 matters for both men and women.
- Myth: “Calcium supplements alone will solve it.” — Truth: Supplements can’t replace exercise, strength training and other habits. Nutrition + movement + lifestyle all matter.
- Myth: “If my bones are already weak, it’s too late.” — Truth: Improvements and slowing of loss are still possible. (Holland Hospital)
Frequently Asked Questions (FAQ)
Q: How much calcium do I really need after 40?
A: For most adults after 40: about 1,000 mg daily; for many women entering menopause or after menopause, about 1,200 mg daily. (El Camino Health)
Q: What if I can’t get much sun for vitamin D?
A: Then dietary sources and/or vitamin D supplements may be required. Talk to your doctor about checking your vitamin D level.
Q: I’m worried about joint pain — can I still do weight-bearing exercise?
A: Yes — you may need to adapt. Low-impact weight-bearing options (brisk walking, elliptical machine, stair climbing) plus resistance training are still very helpful. Consult a physiotherapist or trainer if you have joint issues.
Q: When should I get a bone density scan?
A: While standard guidelines often apply at older ages (e.g., 65+), if you have risk factors (early menopause, steroid use, family history, previous fracture), your doctor may recommend screening earlier. (Penn State Health News)
Q: Can supplements replace exercise and diet?
A: No — supplements are part of the story, but they cannot substitute for physical activity, strength training or lifestyle habits.
Monitoring Progress & Signs to Watch For
- Keep a log of exercise (days per week, types, duration)
- Track dietary intake of calcium, vitamin D, protein
- Monitor weight and general strength (can you do the same lifts/walks as before?)
- Periodically ask your doctor about bone density measurement (if recommended)
- Watch for warning signs: new fractures from low-impact events, back pain (could indicate vertebral fractures), loss of height, increased stoop or curvature of spine
Summary
Improving and maintaining bone health after age 40 involves a comprehensive, multi-factor approach:
- Exercise: weight-bearing, resistance and balance training
- Nutrition: adequate calcium, vitamin D, protein and other bone-supportive nutrients
- Lifestyle: quit smoking, limit alcohol, maintain healthy weight, address fall risk
- Medical / Screening: assess bone density if risk factors exist, consult with provider about therapies
- Home & Environment: safe home setup, fall prevention strategies
Action before significant bone loss occurs helps preserve skeletal strength, reduce fracture risk and support long-term mobility and independence.
Internal Links
- See also our article on Healthy Eating in Midlife
- Also recommended: Strength Training for 40+ Adults
- For balance and fall prevention: Balance Exercises and Older Adults
External Links
- More information from the American Academy of Orthopaedic Surgeons: “Healthy Bones at Every Age” — https://orthoinfo.aaos.org/en/staying-healthy/healthy-bones-at-every-age/ (OrthoInfo)
- Prevention guide from the National Health Service (UK): “Prevention — Osteoporosis” — https://www.nhs.uk/conditions/osteoporosis/prevention/ (nhs.uk)
